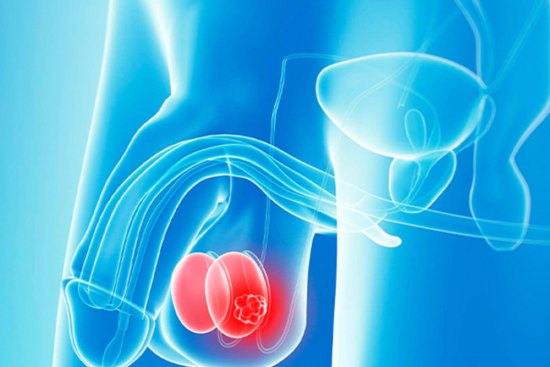
Whether performed for medical reasons, oncological treatment, or gender-affirming purposes, an orchiectomy is a life-changing procedure that requires precision, experience, and personalized care. In Turkey, patients benefit from world-class surgeons, modern hospitals, and a supportive medical tourism service through Turquie Santé.
From your first consultation to post-operative follow-up, our partner clinics ensure safety, confidentiality, and comfort throughout your journey.
Ready to explore your orchiectomy options in Turkey? Request a free medical consultation with Turquie Santé today.